Shortcut to Weight Loss: No Nausea Required
Key Takeaways:
- GLP-1 drugs and nausea: Current weight loss drugs make most people too sick to take them for long. Scientists are looking for better options.
- Appetite-blocking chemical: Researchers found that brain support cells produce a chemical that suppresses appetite, and they created a modified version of this molecule that helped lab animals lose weight without causing illness.
- Brighter drug future: The discovery could lead to better weight loss drugs that skip side effects, like taking a shortcut in a race.
Weight loss and diabetes drugs on the market often do not achieve long-term weight loss for patients. GLP-1 drugs target brain neurons that control appetite but frequently cause side effects. Nausea and vomiting force 70% of patients to stop treatment within a year. Syracuse University chemistry professor Robert Doyle is leading a multidisciplinary team that has identified a different brain target for treating obesity and diabetes, potentially offering weight loss without gastrointestinal distress.
Neurons are the most well-known and obvious target in research and drug development for brain conditions. GLP-1 drugs, for example, target brain neurons in the hindbrain involved in appetite control. But researchers are looking beyond neurons to study “support” cells such as glia and astrocytes that could aid appetite reduction.
A collaborative research effort has revealed that support cells play a role in reducing feelings of hunger, although this process has not been studied in-depth.
“We wanted to know whether support cells might produce new peptides or new signaling molecules that might be critical in body weight reduction,” says Doyle, a medicinal chemist and the Jack and Laura H. Milton Professor of Chemistry in the College of Arts and Sciences at Syracuse University. Doyle is also a professor of pharmacology and medicine at SUNY Upstate Medical University.
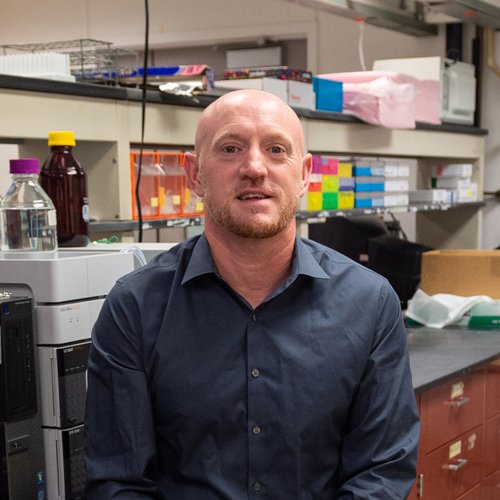
Robert Doyle
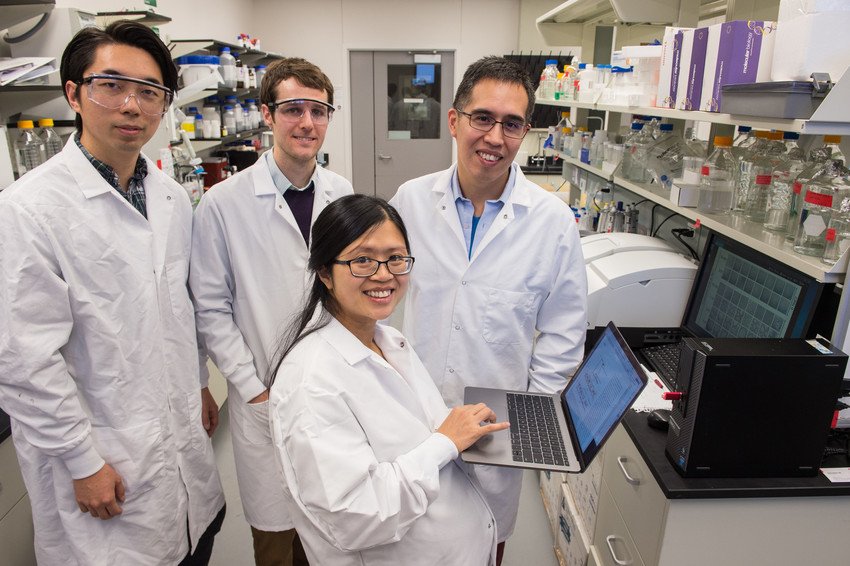
Doyle and his research partners at the University of Pennsylvania and the University of Kentucky identified a chemical created by brain cells called astrocytes that could be key in designing future appetite control drugs without negative side effects. Their study appeared in Science Translational Medicine.
How it works
Think of each brain neuron as a light bulb and support cells as the components that allow the light bulb to brighten, including the wiring, switch and filament.
“All of those supporting parts beyond the light bulb play a role in making the light shine,” says Doyle.
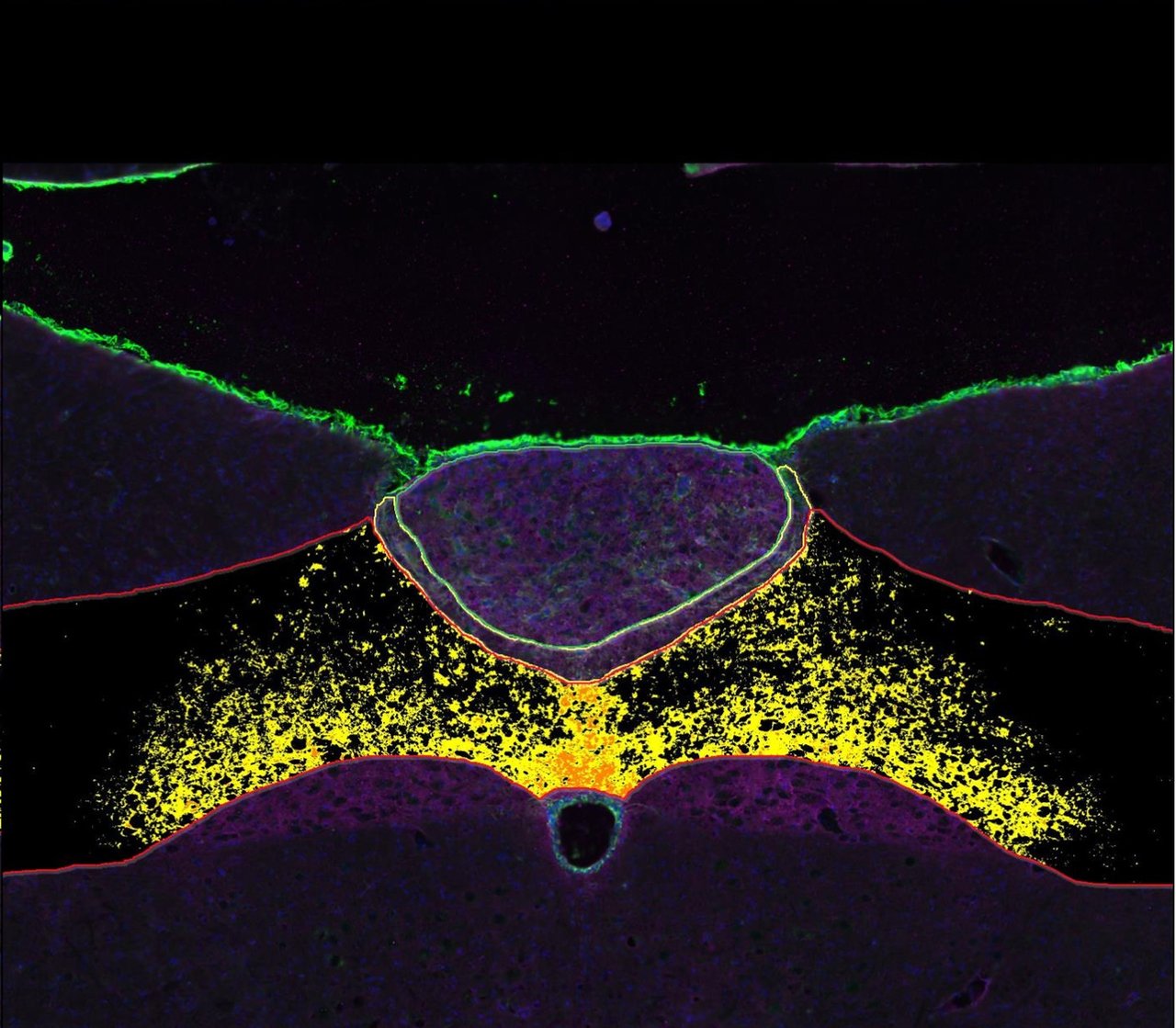
The research team discovered that some support cells in the hindbrain naturally produce a molecule named octadecaneuropeptide (ODN), which suppresses appetite. In lab tests, injecting ODN directly into rats’ brains made them lose weight and improved how they processed glucose.
However, injecting directly into the brain isn’t a practical treatment for people, so researchers created a new version of the molecule named tridecaneuropeptide (TDN). This molecule version could be given to human patients through regular injections akin to today’s Ozempic or Zepbound. When tested in obese mice and musk shrews, TDN helped the animals lose weight and respond better to insulin without causing nausea or vomiting.
Marathon shortcut
One goal of the research team is to produce weight loss without aiming new therapeutic molecules at neurons. The new TDN molecule bypasses neurons, taking a shortcut to directly target neurons’ downstream support cells, which researchers found also produce appetite suppression. TDN cuts short the “marathon” of chemical reactions and negative side-effects caused by GLP-1 drugs.
“Instead of running a marathon from the very beginning like current drugs do, our targeting downstream pathways in support cells is like starting the race halfway through, reducing the unpleasant side effects many people experience,” says Doyle. “If we could hit that downstream process directly, then potentially we wouldn’t have to use GLP-1 drugs with their side effects. Or we could reduce their dose, improving the toleration of these drugs. We could trigger weight loss signals that happen later in the pathway more directly.”
A new company called CoronationBio has been launched to turn this discovery into a real-world treatment. The company has licensed intellectual property related to ODN derivatives for the treatment of obesity and cardio-metabolic disease from Syracuse University and the University of Pennsylvania, with a focus on translating candidates into the clinic. They’re now teaming up with other companies to develop this treatment and aim to start human trials in 2026 or 2027.
Published: July 30, 2025
Media Contact: asnews@syr.edu